Electrical Activity of GIT Smooth Muscle
- Slow waves
- Spike potentials
- Changes of voltage of RMP by other factors
1-Slow waves
These are not action potential. Instead they are slow undulating changes in the resting membrane potential.
-Their intensity: 5-15 mv.
-Their frequency: varies in different parts of the human GIT from 3-12 per minute.
The precise cause of the slow waves is not understood. They do not cause muscle contraction except perhaps in the stomach.
Membrane potentials in GIT smooth muscle
2-Spike potentials
Each time the peaks of the slow waves temporarily become more positive than -40 mv, spike potentials appear on these peaks.
-The cause of these action potential is due to activation of the calcium-sodium channels.
3-Changes of voltage of the RMP
Factors that depolarize the membrane:
1-Stretching of the muscle
2-Stimulating by acetylcholine
3-Stimulation by parasympathetic nerves
4-Stimulation by several specific GI hormones.
Neural Control of GI Functions
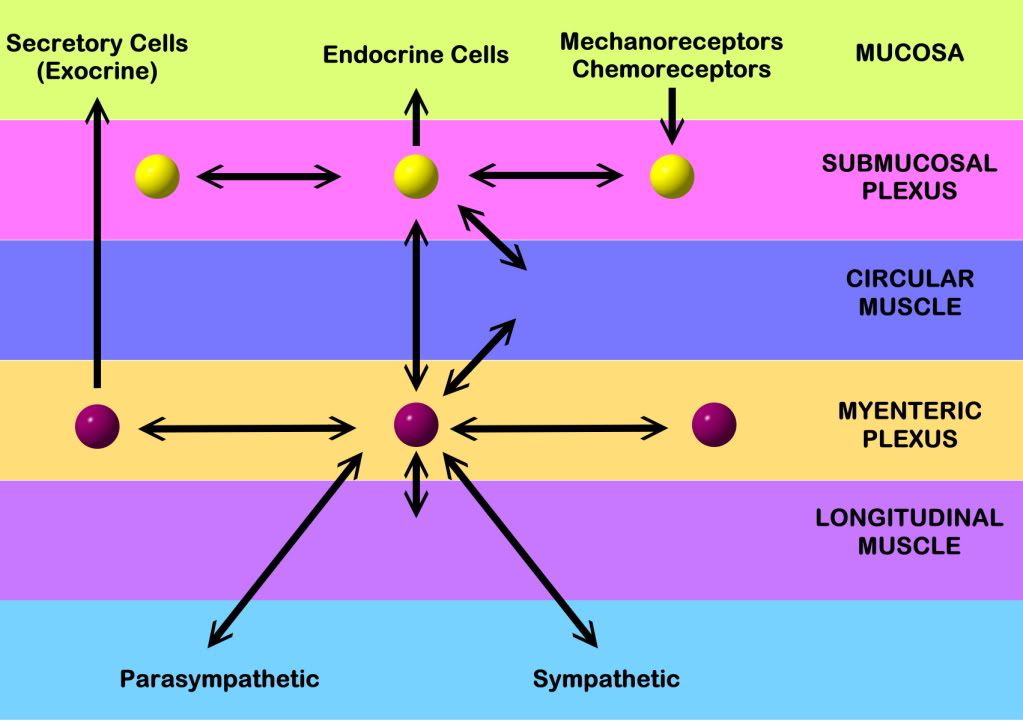
Enteric Nervous System
-Differences between the myenteric and submucosal plexus
-Types of neurotransmitters secreted by enteric nervous system
Control of GI Motility
Autonomic control of GIT:
- Parasympathetic Division
- Sympathetic Division
Hormonal control of Gi Motility
Functional types of Movements
Propulsive Movements
-Peristaltic reflex
-Law of the Gut
-Mass peristalsis
-Antiperistalsis
Mixing Movements
Peristaltic reflex
law of the Gut
1-Esophageal Motility
Types of esophageal motility:
1-primary peristalsis
2-Secondary peristalsis
*Mechanism and function of the lower esophageal sphincter*
2-Gastric Motility
Motor functions of the stomach:
1-Storage function (Receptive relaxation)
2-Mixing function
3-Stomach emptying (Hunger contractions)
Gastric emptying
3-Intestinal Motility
1-Mixing contractions (Segmentation contractions)
2-propulsive movements:
-Peristalsis
-Peristaltic rush
Mixing Movements
Function of the ileocecal valve
A principal function of the ileocecal valve is to prevent backflow of fecal contents from the colon into the small intestine.
4-Colon Motility
1-Mixing movements (Haustrations)
2-Propulsive movements (Mass movements)
3-Defecation
· The central autonomic nervous system (hypothalamus and brain stem) mediates its influence on the gastrointestinal function through the intrinsic, enteric nervous system (the so-called “little brain”).
· Cannons law of the gut: The peristalsis of the small intestine always proceeds in the oral- aboral direction.
· Achlorhydria refers to absence of HCl production in the stomach
· Defaecation is a reflex act involving colon, rectum, anal sphincters and many striated muscles (diaphragm, abdominal and pelvic muscles). The motor pathway is the pelvic nerves. Defaecation implies a temporal release of anal continence brought about by a reflex. The coordinating centre is in the sacral spinal cord.
· Enterogastrones are enterogastric inhibitory hormones liberated from the duodenal mucosa by acid chyme (ie, cholecystokinin: CCK, gastric inhibitory peptide: GIP, secretin, somatostatin, neurotensin and vasoactive intestinal peptide: VIP).
· Haematemesis is defined as vomiting of whole blood or blood clots.
· Incretins are hormones, which increase insulin secretion from the b-cells of the pancreatic islets much earlier and to a greater extent, than when the blood glucose concentration is elevated by intravenous infusion (GIP, glicentin, glucagon-like peptides-1 and -2).
· Intrinsic, enteric nervous system refers to the large number of neuronal connections in the gut wall, in particular the submucosal Meissner plexus,which regulates the digestive glands, and the myenteric Auerbach plexus,primarily connected with gut motility.
· Macrolides are antibiotics, which bind to and prevent translocation on bacterial ribosomes.
· Malabsorption describes the condition resulting from inefficient absorption of nutrients by the gastrointestinal tract.
· Melaena is defined as passage of dark tarry stools (coal-black, shiny, sticky, and foul smelling).
· Migrating motor complex refers to a gastric sequence of events, where contractions occur each 90 min during fasting. There is a quiet period (I) followed by a period of irregular contraction (II), and culminated with aperistaltic rush (III) accompanied by increased gastric, pancreatic and biliary secretion.
· NANC neurons are non-adrenergic, non-cholinergic postganglionic neurons, which liberate gastrin-releasing peptide (GRP) to the gastrin producing G-cells.
· Nitric oxide (NO) is a possible neurotransmitter between the preganglionic and the NANC postganglionic neurons.
· Paracrine secretion is the release of signal molecules to neighbour cells.
· Peptide hormone families are groups of hormones that exhibit sequence homology: They possess a common amino acid sequence, such as thegastrin family, which has sequence homology in their terminal penta-peptide. Peptide hormones have autocrine and paracrine functions in the gastrointestinal tract.
· Peristalsis is a propagating contraction of successive sections of circular smooth muscle preceded by a dilatation. The dilatated intestinal wall is drawn over its content in this reflex mechanism, which transports the content aborally and is called the law of the gut.
· Segmentation divides the small intestine into many segments by localised circular smooth muscle contractions. Segmentation mixes the intestinal content and propagate it at a slow rate, which allows sufficient time for digestion and absorption.
· Slow waves (basic electrical rhythm) are slow gastrointestinal depolarisation’s occurring at a frequency of 3-18 per min. The slow waves change the resting membrane potential of smooth muscles from -50 to -40 mV.
· Spike potentials are periodic fast waves of depolarisation that most often follow a slow wave, and then always initiate gastric contractions (elicited by a rise in cytosolic [Ca2+]).
· Vaso-active intestinal peptide (VIP) is a vasodilatator in line with adenosine, ATP, NO. The increased bloodflow increases intestinal secretion.